Life Science Washington’s Member Spotlight series highlights the innovations, impact, and future vision of our member companies in the life sciences industry. Through curated questions, we explore their origins, breakthrough technologies, local presence, and industry leadership. This initiative showcases their contributions and strengthens connections within the life sciences community. If your organization is a member and would like to be highlighted in a future spotlight, please contact Kaitlyn Campitiello, Director of Marketing and Communications.
Tell us your origin story. How did Benaroya Research Institute (BRI) come to be, and what inspired its creation.

The Virginia Mason Research Center, which later became Benaroya Research Institute, was established in 1956. It was founded by the leadership of Virginia Mason Medical Center with the vision of enhancing healthcare through research. Our early work included helping develop the first insulin pumps, innovations in hyperbaric medicine, and pioneering research in immunology.
In the 1980s, BRI’s focus on immune system diseases gained momentum under Dr. Jerry Nepom. This led to a transformational gift from the Benaroya family to support our type 1 diabetes (T1D) research program in 1987. In the years that followed, our teams developed groundbreaking tools to better understand genes and cells that play a vital role in the immune system, including the development of MHC Class II tetramers by Dr. Bill Kwok, a tool that revolutionized immune cell research.
At the turn of the century, BRI continued to grow, building the infrastructure to transform our lab discoveries into life-changing care. BRI expanded clinical research programs, built robust biorepositories, and played a leading role in autoimmune disease trials. In 2019, we launched a bold new mission: to predict, prevent, reverse and cure immune system diseases. BRI played a key role in developing and testing teplizumab, the first ever drug to delay the onset of T1D and any autoimmune disease. Our ongoing work focuses on improving screening and prevention for a wide variety of immune system diseases and developing more targeted therapies with fewer side effects — moving closer to our vision of a healthy immune system for everyone.
Can you share some of the most groundbreaking discoveries made at BRI? How have these discoveries impacted the broader scientific community?
BRI has played a key role in many groundbreaking discoveries that impact the broader scientific community and improve the lives of people with immune system diseases, including:
- Discovery of the HLA-DQ Beta Gene, a major breakthrough in understanding the genetic basis of type 1 diabetes.
- Pioneering MHC Class II Tetramers, which allow scientists to find and isolate immune system cells. This breakthrough allows scientists to identify very specific cells and study how they trigger immune responses.
- Discovery of the Th2A cell, a promising target for peanut allergies and all types of allergies.
- Playing a leading role in detailing the stages of type 1 diabetes. This paved the way to predicting disease onset and the first-ever therapy to delay the onset of T1D and any autoimmune disease. BRI is now working toward similar advances in other autoimmune diseases.
Improving our overall understanding of the immune system through a number of studies including the Sound Life Project. This study aims to paint a detailed picture of the immune system in health and to improve our understanding of which immune system changes are normal and which ones are related to disease.
People with autoimmune disease are known to have deficiency in frequency, function, or responsiveness to regulatory T cells (Tregs). BRI’s long-standing research in this area has influenced and informed many projects specifically around FOXP3. FOXP3, known as the “master regulator” of Tregs, has been a foundational element of multiple research projects at BRI. Our scientists had earlier observed that there are two versions, or isoforms, of FOXP3, which were expressed equivalently in Tregs from healthy people. We have now found that the smaller isoform, which is less functional, is found at a higher ratio in patients with lupus. Given FOXP3’s involvement in regulatory t-cells, this discovery could have implications across multiple autoimmune diseases.
How does BRI collaborate with other research institutions and organizations? Can you share examples of successful partnerships and their outcomes?
BRI has many successful partnerships with other organizations:
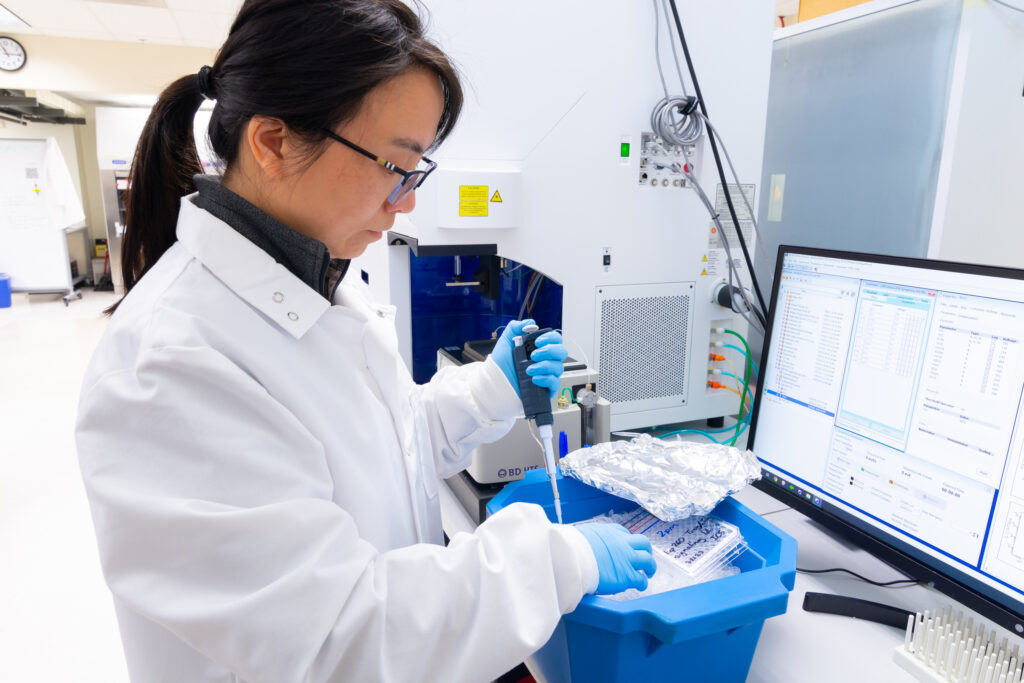
- One important way BRI fulfills our mission to advance the science to predict, prevent, reverse and cure immune system diseases is through our biorepositories. We share resources and expertise to help scientists across the world answer important questions about immune system diseases. Our biorepositories are a vital resource that has led to countless discoveries with many more on the horizon. They hold more than 350,000 samples from over 16,000 participants. We distribute more than 1,400 samples to external collaborators every year. We also have a dedicated team that educates people about participating in research and recruits and manages participants. They ensure that samples are collected and stored properly leading to the highest quality samples and data.
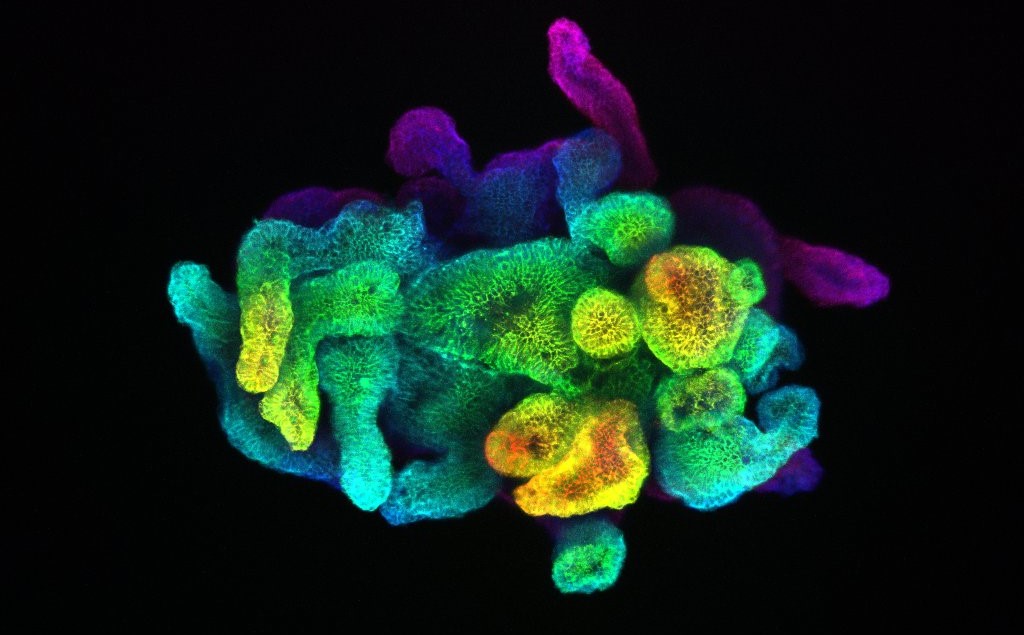
- BRI’s CORE labs support scientists both inside and outside the institute. While each of the labs’ purposes, staff and technologies are different, they are each rooted in BRI’s work to advance science to improve human health. This translates into each core lab collaborating to provide the best possible outcome for projects. Our Human Immunophenotyping core is particularly interested in sharing their expertise and supporting researchers in robust, reproducible assays for application to precious human samples. This includes study design and training on new technologies to execution, data analysis and interpretation.
- Our CORE Labs include expertise in:
- Imaging
- Histology
- Flow cytometry
- Genomics and bioinformatics
- Tetramers
- Human Immuno Phenotyping
- BRI has a longstanding partnership with Seattle Children’s Research Institute (SCRI), where BRI’s Dr. Jane Buckner and SCRI’s Dr. David Rawlings are pioneering regulatory T cells as a potential treatment for type 1 diabetes. This approach aims to target the root cause of T1D by turning the cells that cause T1D into cells that can protect you from T1D. If this approach proves successful in T1D, it could also be a game-changing treatment for other autoimmune diseases.
- BRI leads the Immune Tolerance Network (ITN), a collaborative network for clinical research, funded by the National Institute of Allergy and Infectious Diseases, part of the National Institutes of Health (NIH). The ITN develops and conducts clinical trials, each supported by mechanistic studies, of specialized immune tolerance therapies in autoimmune diseases, allergies, asthma and organ transplantation.
- BRI is a key player in the Human Immunology Project Consortium, a network of researchers studying the human immune system. Using advanced tools, they analyze how the immune system responds to infections, vaccines, and treatments. Their work helps scientists better understand immunity and improve vaccine safety and effectiveness.
- BRI has a robust collaborative research portfolio and is involved in many industry-sponsored clinical trials.
How has BRI seeded new ventures, such as GentiBio? How do these spinouts enhance BRI’s research goals, and what can we expect in the future?
Because of BRI’s singular focus in immune-disease and pathways, BRI researchers have significant expertise in pathways that are of interest to drug developers. For example, BRI’s research interest in Tregs and antigen-specific T cells led to the development (with SCRI) of intellectual property that was spun into GentiBio. BRI is actively considering other commercialization opportunities that partner our know-how and technology with others (entrepreneurs, companies and investors) to develop new therapies to prevent, reverse and, eventually, cure immune-mediated diseases.

How does BRI engage with patients and the broader community to raise awareness about autoimmune diseases and the importance of research participation? What initiatives or programs have been particularly impactful?
BRI’s team often engages with local disease-related organizations to help raise funds and awareness. This includes participating in the 321 Buddy Walk for Down Syndrome and Breakthrough T1D’s Beat the Bridge.
We have a close partnership with Virginia Mason Medical Center, where many doctors are co-investigators on BRI studies and biorepositories. This partnership has led many patients to donate samples to our biorepositories which include 11 research areas, over 16,000 participants and more than 350,000 samples.

Last year we were excited to host our first annual BRI Immunology Symposium: New Horizons in Immunity and Disease to bring together leading voices from the local and national immunology research community for a day of collaboration, learning, discussion and networking. Seattle is a hub for immunology research and we are excited to promote this through this annual event. This year’s symposium will take place on Monday, April 28 and already has a great line-up of national speakers.
Where do you see BRI in the next 5-10 years? Can you share some of BRI’s most exciting upcoming projects or innovations?

In the next five to ten years, two core focuses will be advancing our work in screening and prevention and developing more targeted therapies with fewer side effects for immune system diseases. We have many exciting projects and innovations on the horizon including:
- Bringing screening for autoimmune diseases into primary care. While early screening for cancer and heart disease is common, screening for autoimmune disease has not been widely available. BRI’s team is working to bring these screenings into clinical care with the vision of helping people better understand their risk, start treatment early, and reduce the risk of dangerous complications like diabetic ketoacidosis.
- Advancing precision medicine. BRI is on the leading edge of precision medicine in immune system diseases and on a mission to better define the right therapy for the right person at the right time.
- Through our Center for Translational Immunology, we will continue to build on discoveries made by scientists in the Center for Fundamental Immunology, looking for patterns and further testing their theories in human samples. We’ll also continue and expand our work in populations at higher risk for autoimmune disease, such as women and people with Down syndrome.
- Exploring how environmental factors like air quality, diet and wildfire smoke impact the development and progression of autoimmune diseases.
Learn more about Benaroya Research Institute and stay updated by following their social channels:
- BRI Website: https://www.benaroyaresearch.org/
- BRI Career Site: https://www.benaroyaresearch.org/careers
- Socials:
If your organization is a member of Life Science Washington and would like to be highlighted in a future spotlight, please contact Kaitlyn Campitiello, Director of Marketing and Communications.